Integrated Mental Health Care

Introduction to Holistic Healthcare at Incontact Counselling
The body is a host of interconnected systems. The broad range of mental health issues we deal with have a strong physiological link. Emotions can manifest as physiological symptoms—nerves are felt as butterflies in the stomach, guilt as a pinch in the gut, joy as a total lightness of the body, heartburn for anger and heartache for melancholia. Most prominently, stress can manifest as migraines, aches or fatigue. Taking into account that our mind and body are not mutually exclusive, the integrative approach to healthcare is necessary for more effective healing.
The body thrives off balance. When one system is attacked, the others go down as well. For example, major contributing factors to mental health are nutritional deficiencies, sleep and diet. Likewise, all of these problems are interconnected. Holistic approaches to healthcare aims to support your wellbeing by considering your physical, emotional, social and spiritual needs as an interaction, rather than each element in isolation.
The Gut-Brain Axis
A web of literature has boiled down to one fine point: the mind has immense influence over our gut microbiota, and vice versa. The gut-brain axis is one of many links, and is a direct contributor to our mental health. The gastrointestinal tract houses a biome of microorganisms that interact with the central nervous system through the immune system, and synthesise neurotransmitters such as dopamine, serotonin and γ-aminobutyric acid (GABA), which influence our mood (Sharon et al., 2016).
95% of our body’s serotonin is produced in the gut (Terry & Margolis, 2016). Serotonin modulates “brain development, sleep, mood, appetite, and temperature regulation”. An imbalance of gut serotonin may impair brain function. In the pink of health, this microbe ecosystem harmoniously supports intestinal health, energy production and immune system function. Yuan et al. (2021) reports that over 50% of patients with inflammatory bowel disease had depression and anxiety. Upsetting the balance of gut-microbiota impacts neurotransmitter production, and low levels of serotonin have been implicated in symptoms of anxiety, sleep problems, digestion, and mood disorders. Changes to one system may influence the others in a sequential chain of responses. Stress can aggravate inflammation by changing the composition of gut microbiota, thus affecting our mental health. The vicious cycle runs over and over again. To heal, we must break this inflammatory cycle.
As such, the integrative approach to healthcare—partnering functional medicine and counselling—can leverage the interconnecting link between the gut and the brain, and deliver more protective treatment. By healing your gut, you can heal your mind, and vice versa. Our counsellors collaborate with functional medicine specialists to restore your gut-brain axis, and guide you toward better health.
Sleep and Mental Health
Experts recommend that adults acquire 7 to 8 hours of quality sleep per night. Any less negatively influences mood, memory and concentration. Research shows that children with sleep disorders present with 1.5 times the likelihood of developing depression symptoms than children without (Sivertsen et al., 2020). Sleep deprivation can impact a person’s development on a molecular level, such as inhibiting regulation of GABA receptors, thus disrupting signalling within those pathways, which are essential for memory consolidation processes. Stressful life events affect immune response, digestion, mood, and energy storage (Smith & Vale, 2006), thus affecting our ability to sleep. Sleep deprivation influences the immune and digestive systems, which may lead to neuroinflammation, which has been associated with mood disorders (Li et al., 2019).
Improving the quality of sleep through therapeutic interventions has been suggested to reduce depression, anxiety, and stress (Scott et al., 2021). Holistic approaches to healthcare acknowledges the complex links between physical and mental health. At Incontact Counselling, we work with health coaches to assess sleep issues, and work with our counsellors to formulate treatment plans that can help you build the skills required for a healthy mind and a good night’s rest.
Physical Exercise and Mental Health
Exercise is important to maintaining physical and mental health. Health experts prescribe at least 150 minutes of moderate to vigorous physical exercise per week. Exercise can regulate hormones and neurotransmitters to protect the body from the negative impacts of psychological distress. The benefits of exercise extend to promoting neurogenesis, plasticity and increasing the brain’s oxygen supply, which leads to increased mood (Vecchio et al., 2018). Aerobic exercise can positively regulate dopamine and serotonin through increased brain blood flow (Lin & Kuo, 2013). During exercise, our muscles release a hormone called irisin that plays a protective role in the central nervous system, and is sensed by the brain. Exercise also supports maintenance of structural brain integrity, supporting brain regions responsible for cognition and memory. Exercise is also associated with improvements in sleep quality, mood, quality of life, and various psychiatric disorders (Alnawwar et al., 2023). It is also suggested to help manage addiction by alleviating substance cravings.
The benefits of exercising regularly are abundant, especially for supporting our mental functions and physical health. So if we see a client who is struggling to have physical activity incorporated in their schedule, we know it will have a significant impact on their mental health. As these contribute to maintaining good psychological health. At Incontact Counselling, we curate and work with you to facilitate gentle changes towards physical movement. We also work with health coaches who work closely with you to incorporate changes.
Holistic Approach to Healthcare at Incontact Counselling
Taken together, these interconnected links between physical and mental health provide evidence-based support for holistic approaches to healthcare here at Incontact Counselling. Cross-examination of other aspects of health—the gut microbiome, sleep quality and fitness—with regard to psychological health may maximise the healing process. The integrative care of GPs, health coaches, and counsellors can provide a well-rounded perspective on your health.
At Incontact Counselling, our holistic healthcare team blankets you with the best care possible. With the growing dearth of evidence that links our psychological health with our body’s biological systems, we are compelled to bring integrative healthcare to the forefront of our services. We currently have an in-house health coach, Kavita, who will journey with you to make behavioural changes that contribute to your mental & physical wellbeing.
Alhola, P., & Polo-Kantola, P. (2007). Sleep deprivation: Impact on cognitive performance. PubMed. https://pubmed.ncbi.nlm.nih.gov/19300585
Alrousan, G., Hassan, A., Pillai, A. A., Atrooz, F., & Salim, S. (2022). Early life sleep deprivation and brain development: insights from human and animal studies. Frontiers in Neuroscience, 16. https://doi.org/10.3389/fnins.2022.833786
Alnawwar, M. A., Alraddadi, M. I., Algethmi, R. A., Salem, G. A., Salem, M. A., & Alharbi, A. A. (2023). The Effect of Physical activity on sleep quality and sleep Disorder: A Systematic review. Curēus. https://doi.org/10.7759/cureus.43595
Appleton, J. (2018). The Gut-Brain Axis: Influence of microbiota on mood and mental health. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6469458/
Arvidson, E., Dahlman, A. S., Börjesson, M., Gullstrand, L., & Jonsdottir, I. H. (2020). The effects of exercise training on hypothalamic-pituitary-adrenal axis reactivity and autonomic response to acute stress—a randomized controlled study. Trials, 21(1). https://doi.org/10.1186/s13063-020-04803-3
Brummelte, S., Glanaghy, E. M., Bonnin, A., & Oberlander, T. (2017). Developmental changes in serotonin signaling: Implications for early brain function, behavior and adaptation. Neuroscience, 342, 212–231. https://doi.org/10.1016/j.neuroscience.2016.02.037
Erickson, K. I., Leckie, R. L., & Weinstein, A. M. (2014). Physical activity, fitness, and gray matter volume. Neurobiology of Aging, 35, S20–S28. https://doi.org/10.1016/j.neurobiolaging.2014.03.034
Felger, J., & Lotrich, F. (2013). Inflammatory cytokines in depression: Neurobiological mechanisms and therapeutic implications. Neuroscience, 246, 199–229. https://doi.org/10.1016/j.neuroscience.2013.04.060
Foster, J. A., Baker, G. B., & Dursun, S. M. (2021). The relationship between the gut Microbiome-Immune System-Brain axis and major depressive disorder. Frontiers in Neurology, 12. https://doi.org/10.3389/fneur.2021.721126
Ge, L., Liu, S., Li, S., Yang, J., Hu, G., Xu, C., & Song, W. (2022). Psychological stress in inflammatory bowel disease: Psychoneuroimmunological insights into bidirectional gut–brain communications. Frontiers in Immunology, 13. https://doi.org/10.3389/fimmu.2022.1016578
Han, W., Tellez, L. A., Perkins, M. H., Perez, I. O., Qu, T., Ferreira, J., Ferreira, T. L., Quinn, D., Liu, Z., Gao, X., Kaelberer, M. M., Bohórquez, D. V., Shammah-Lagnado, S. J., De Lartigue, G., & De Araujo, I. E. (2018). A neural circuit for Gut-Induced reward. Cell, 175(3), 665-678.e23. https://doi.org/10.1016/j.cell.2018.08.049
Institute of Medicine (US) Committee on Sleep Medicine and Research; Colten HR, Altevogt BM, editors. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington (DC): National Academies Press (US); 2006. 3, Extent and Health Consequences of Chronic Sleep Loss and Sleep Disorders. Available from: https://www.ncbi.nlm.nih.gov/books/NBK19961/
Kasarello, K., Cudnoch-Jedrzejewska, A., & Czarzasta, K. (2023). Communication of gut microbiota and brain via immune and neuroendocrine signaling. Frontiers in Microbiology, 14. https://doi.org/10.3389/fmicb.2023.1118529
Kumar, A., Pramanik, J., Goyal, N., Chauhan, D., Sivamaruthi, B. S., Prajapati, B. G., & Chaiyasut, C. (2023). Gut microbiota in Anxiety and Depression: Unveiling the relationships and management options. Pharmaceuticals, 16(4), 565. https://doi.org/10.3390/ph16040565
Li, X., Liang, S., Li, Z., Li, S., Xia, M., Verkhratsky, A., & Li, B. (2019). Leptin increases expression of 5-HT2B receptors in astrocytes thus enhancing action of fluoxetine on the depressive behavior induced by sleep deprivation. Frontiers in Psychiatry, 9. https://doi.org/10.3389/fpsyt.2018.00734
Li, Y., Gu, S., Wang, Z., Li, H., Xu, X., Zhu, H., Deng, S., Ma, X., Feng, G., Wang, F., & Huang, J. H. (2019). Relationship between stressful life events and sleep quality: rumination as a mediator and resilience as a moderator. Frontiers in Psychiatry, 10. https://doi.org/10.3389/fpsyt.2019.00348
Lin, T., & Kuo, Y. (2013). Exercise benefits brain function: the monoamine connection. Brain Sciences, 3(4), 39–53. https://doi.org/10.3390/brainsci3010039
Mittal, R., Debs, L. H., Patel, A. P., Nguyen, D., Patel, K., O’Connor, G., Grati, M., Mittal, J., Yan, D., Eshraghi, A. A., Deo, S. K., Daunert, S., & Liu, X. Z. (2017). Neurotransmitters: the critical modulators regulating Gut–Brain axis. Journal of Cellular Physiology, 232(9), 2359–2372. https://doi.org/10.1002/jcp.25518
Schramm, E., & Waisman, A. (2022). Microglia as central protagonists in the chronic stress response. Neurology® Neuroimmunology & Neuroinflammation, 9(6). https://doi.org/10.1212/nxi.0000000000200023
Scott, A. J., Webb, T. L., James, M. M., Rowse, G., & Weich, S. (2021). Improving sleep quality leads to better mental health: A meta-analysis of randomised controlled trials. Sleep Medicine Reviews, 60, 101556. https://doi.org/10.1016/j.smrv.2021.101556
Sharma, A., & Sharma, V. (2023). The Gut-Brain Connection: A case report on depression in Ulcerative colitis and Novel Treatment approach. Curēus. https://doi.org/10.7759/cureus.48462
Sharon, G., Sampson, T. R., Geschwind, D. H., & Mazmanian, S. K. (2016). The Central Nervous System and the Gut Microbiome. Cell, 167(4), 915–932. https://doi.org/10.1016/j.cell.2016.10.027
Sivertsen, B., Harvey, A. G., Reichborn‐Kjennerud, T., Ystrom, E., & Hysing, M. (2020). Sleep problems and depressive symptoms in toddlers and 8‐year‐old children: A longitudinal study. Journal of Sleep Research, 30(1). https://doi.org/10.1111/jsr.13150
Smith, S. M., & Vale, W. W. (2006). The role of the hypothalamic-pituitary-adrenal axis in neuroendocrine responses to stress. Dialogues in Clinical Neuroscience, 8(4), 383–395. https://doi.org/10.31887/dcns.2006.8.4/ssmith
Terry, N., & Margolis, K. G. (2016). Serotonergic mechanisms regulating the GI tract: experimental evidence and therapeutic relevance. In Handbook of experimental pharmacology (pp. 319–342). https://doi.org/10.1007/164_2016_103
Thursby, E., & Juge, N. (2017). Introduction to the human gut microbiota. Biochemical Journal, 474(11), 1823–1836. https://doi.org/10.1042/bcj20160510
Vecchio, L. M., Meng, Y., Xhima, K., Lipsman, N., Hamani, C., & Aubert, I. (2018). The neuroprotective effects of exercise: Maintaining a healthy brain throughout aging. Brain Plasticity, 4(1), 17–52. https://doi.org/10.3233/bpl-180069
Yuan, X., Chen, B., Duan, Z., Xia, Z., Ding, Y., Chen, T., Liu, H., Wang, B., Yang, B., Wang, X., Liu, S., Zhou, J., Liu, Y., Wang, Q., Shen, Z., Xiao, J., Shang, H., Liu, W., Shi, G., . . . Chen, Y. (2021). Depression and anxiety in patients with active ulcerative colitis: crosstalk of gut microbiota, metabolomics and proteomics. Gut Microbes, 13(1). https://doi.org/10.1080/19490976.2021.1987779
Zhang, J., Li, X., Tang, Z., Xiang, S., Tang, Y., Hu, W., Tan, C., & Wang, X. (2024). Effects of stress on sleep quality: multiple mediating effects of rumination and social anxiety. Psicologia, 37(1). https://doi.org/10.1186/s41155-024-00294-2
Zhang, T., Wang, K., Li, N., Hurr, C., & Luo, J. (2021). The Relationship between Different Amounts of Physical Exercise, Internal Inhibition, and Drug Craving in Individuals with Substance-Use Disorders. International Journal of Environmental Research and Public Health/International Journal of Environmental Research and Public Health, 18(23), 12436. https://doi.org/10.3390/ijerph182312436
Zhang, Y., Zhang, X., & Lin, S. (2022). Irisin: A bridge between exercise and neurological diseases. Heliyon, 8(12), e12352. https://doi.org/10.1016/j.heliyon.2022.e12352
Submit a Comment
Your email address will not be published. Required fields are marked *
Recent Blogs
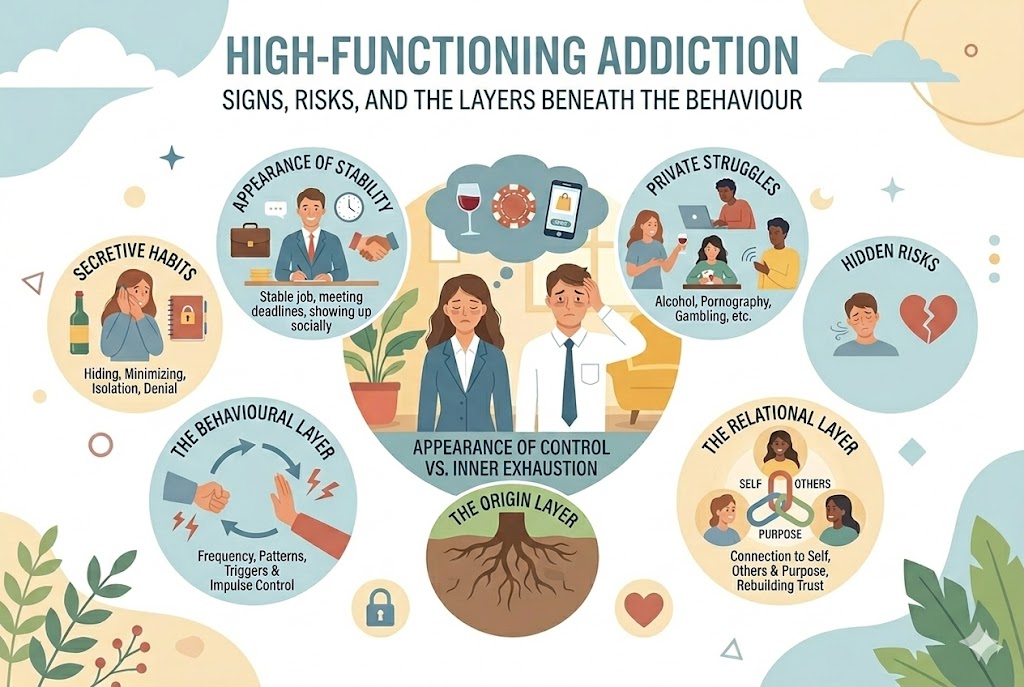
High-Functioning Addiction: Signs, Risks, and the Layers Beneath the Behaviour
5 March, 2026
Addiction isn’t always visible. Some individuals continue to work, parent, meet deadlines, and show up socially – all while privately struggling wi...
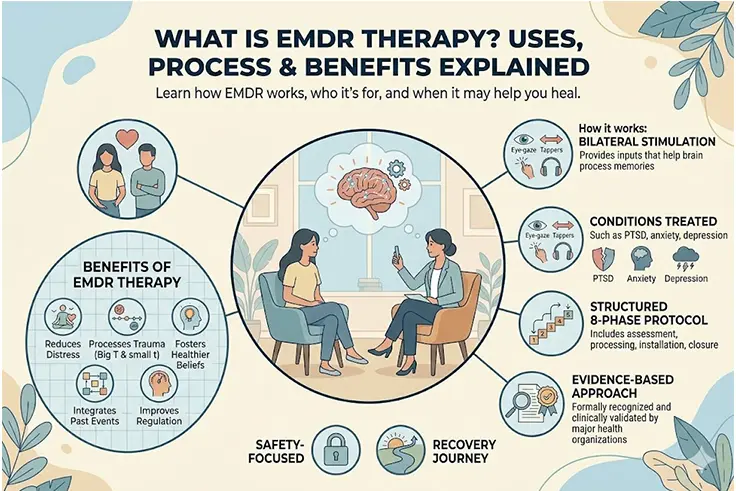
What Is EMDR Therapy? Uses, Treatment & Benefits Explained
2 March, 2026
What is EMDR therapy? EMDR (Eye Movement Desensitisation and Reprocessing) therapy is an evidence-based approach that helps individuals process and heal fr...
What to Do When Your Partner Refuses Couples Therapy
6 February, 2026
When a partner refuses couples therapy or a partner doesn’t believe in therapy, it can leave you feeling stuck, alone, and carrying the emotional weight ...